In healthcare, executive teams face a pivotal decision: forge a path of innovation or remain stagnant. In some health systems, remaining stagnant means clipped growth opportunities, access and capacity issues, unfavorable workforce retention, poor staff utilization, and excessive premium costs of labor.
In the dawn of AI, a fresh dialogue on the economic value of nursing, and at a time where unit managers are being asked to do more, and more – workforce retention, quality of care, and fiscal sustainability are each threatened.
Over the next few paragraphs, we discuss how the emerging discipline of health workforce optimization, particularly the staff scheduling sciences, not only underpin operational success but also catalyze innovation within healthcare settings.
At the core of this article is the perspective that the central trigger to innovation and the subsequent rewards is (a) the empowerment of unit managers and their enablement to perform as catalysts for change, which (b) relies on providing service models and supports that put the manager at the center.
Unit leaders are typically skilled clinicians who have excelled at their craft and are subsequently made in charge of a business unit, clinical, and administrative functions. Unit leaders are responsible for a tremendous number of critical functions. Of particular importance in this discussion is the provision of institutional processes organized to alleviate time spent on all-encompassing, transactional, staff scheduling and deployment ecosystem.
A discussion on staff scheduling service models and the required strategic functions nested in a nurse manager support framework sets the stage for senior leaders to reflect on the kind of healthcare organization they aspire to be.
The Decision: What Type of Organization Do You Want to Be?
Across health leaders, CEOs, CFOs, CNOs, CHROs, and COOs, confront fundamental questions: Does our organization embody innovation, or are we stuck “in a rut,” doing things the way that we have always done them, even if we know they can be done better? Do the “lean teams” who visit units to identify efficiencies have a coordinated strategic agenda, or are they deployed towards ad-hoc improvements? Do we empower managers to lead or tie them down with too many repetitive transactional duties? How do we make our values come alive each and every day for our teams?
These types of questions are critical to ask right now because margins are thin, and deploying the right skill in the right place at the right cost is always a challenge. Staff scheduling, typically viewed as low value, is rising on the strategic agenda. This is especially true since the pandemic shone a light on this ecosystem as very emotional for staff, critical to enable care, and today, on the heels of many scheduling/timekeeping software systems implementations gone awry.
Innovative healthcare requires unit managers to be supported by the organization, and there must be a degree of agility in workforce scheduling. Proactive planning, prioritizing staff wellness, and empowering managers with the capacity to lead effectively. Linking workforce optimization with innovation is not just strategic; it’s crucial for operational efficiency, long-term success, retention, and quality of care.
The Link Between Unit Leader Capacity and Operational Challenges
Operational challenges in healthcare often stem from—or are exacerbated by—underlying workforce capacity utilization issues. Common symptoms include the overuse of agency staff, high turnover rates, and increased burnout, all of which can diminish patient safety and satisfaction. Introducing strategic “capacity management” as a cornerstone of workforce optimization can shift managers from reactive to proactive stances, thus addressing these challenges and improving overall operational health.
Unit Managers: Putting Leaders at the Center
Unit leaders play a vital role in the efficiency and effectiveness of healthcare operations, particularly through their influence on scheduling and deployment. However, they often face immense pressures from outdated processes that hinder their operational potential. In many organizations, we ask managers to build schedules and to fill shifts. Although critical tasks from the perspective of operationalizing the intended model of care, a mix of skills and budget, these essentially are transactional, repetitive tasks.
Innovative organizations recognize the importance of re-engineering these processes to alleviate stress and enhance managers’ ability to lead and focus on quality and their teams by being closer to the point of care. Supports need to be in place for operational leaders. In a time when retention is paramount, it is these leaders who ultimately assume the clinical and financial risks of scheduling and deployment decisions yet should not be consumed with transactional scheduling decisions.
Traditional workforce processes in healthcare are typically inflexible and reactive, often triggered in the short term, which undermines the efficiency and morale of staff. Much is left to the manager’s knowledge, skill, and abilities in this complex arena, which, in addition to taking time away from innovation, creates inconsistencies, inequity, and a lack of standardization, differing from unit to unit and site to site.
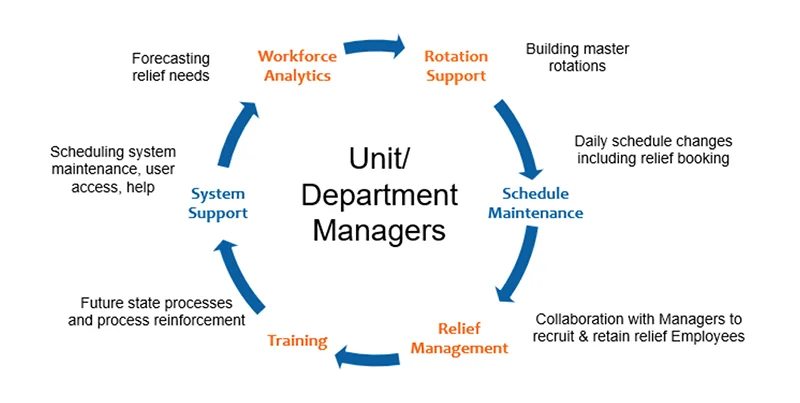
Figure 1.0 above presents a support framework for frontline leaders which pulls staff scheduling from the basement into a strategic Workforce Optimization business unit that can effortlessly operationalize and deploy the intended model of care, skill, position mix, and budget each shift each day while taking advantage of predictable baseline needs and dips and surges in census, acuity and other patterns AI and other analytics can identify and inform.
Establishing a robust staff scheduling ecosystem by optimizing schedules, processes, backfill strategies, and service models creates automation in decision-making, shift filling, and analytics.
Operational Benefits of Smarter Workforce Optimization
In order to capture benefits, the design of this ecosystem must incorporate data-driven decision-making, interdepartmental collaboration, leverage the predictability that does exist in operations, and tap into real-time capacity data. The benefits are manifold, including reduced stress for unit managers and improved outcomes for staff and patients alike.
The tangible benefits of smarter workforce optimization include:
- Reduced overtime costs
- Decreased reliance on agency staff
- Enhanced employee retention and recruitment
- Streamlined compliance with staffing regulations
Additionally, optimized processes contribute to improved patient safety and care quality while ensuring compliance with staffing regulations. These improvements underscore the importance of choosing to be an innovative organization.
Introducing the Workforce Edge Model
The Workforce Edge’s Model of Health Workforce Optimization © offers a proven, comprehensive solution to the challenges of planning, scheduling, and deploying the healthcare workforce. Tried, tested, and refined over two decades of application across the continuum of care private and not-for-profit systems in the United States, Canada, Australia, and Europe, the model is built on comparative advantage. By aligning the model to the cultural context, priorities, and current staff scheduling maturity, your organization can establish or improve strategic staff scheduling support. Workforce Edge enables healthcare leaders to align workforce processes with broader operational goals.

Innovation in healthcare begins with creating space for the frontline. To do so, rethinking how workforce optimization can transform leadership and redefine organizational practices is the starting point. The Workforce Edge model stands out as a transformative solution for healthcare organizations aiming to innovate and optimize their workforce. We invite you to visit workforce-edge.com to discover how our model can empower your unit managers and elevate your organization’s performance.
